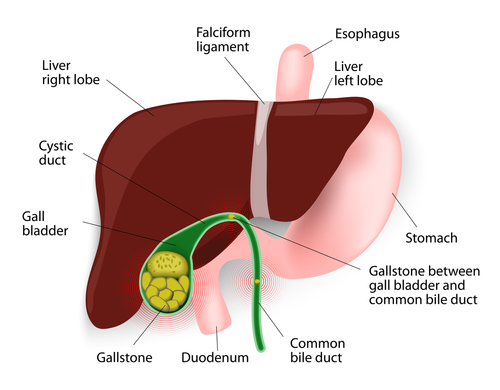
Many of us have occasionally experienced heartburn (which to clarify, has nothing to do with the heart), whether after Thanksgiving dinner or by lying down too soon after eating. If repeated bouts of “heartburn” or sour-tasting fluid in your throat have affected you, however, these are typical symptoms of a common health issue called gastroesophageal reflux disease (“GERD”), also referred to as reflux.
GERD is caused by acid escaping from the top of the stomach through a weakened one-way valve, and flowing backwards as far as the throat. To help ease symptoms, non-operative treatment such as the use of over-the-counter antacids, increasing exercise, placing a foam wedge at the head of the bed and prescription medication can be effective. If these and any other methods recommended by your physician do not provide relief, it may be necessary to consider surgical correction of this very manageable condition.
Surgical Care to Relieve GERD
GERD indicates the one-way valve between the esophagus and the stomach, called the lower esophageal sphincter (“LES”), is weakened and requires structural support. The condition can occur in patients of any age, from infants to mature adults.
Correcting GERD means repairing the LES. Typically repaired by minimally invasive laparoscopic surgery, surgeons recreate the LES by wrapping the very top of the stomach around the lower part of the esophagus. This correction allows the LES to close immediately after food passes through to the stomach, keeping acids intact.
Recovery from LES Surgery
Most LES repair surgeries occur via minimally invasive laparoscopic surgery. As we’ve shared in the previous blog What Is Minimally Invasive Surgery?, this type of surgery helps patients leave the hospital and return to work sooner due to the small keyhole incisions made during the procedure. Generally, when LES repair is performed via minimally invasive laparoscopic surgery, patients can expect to go home 1 to 3 days after surgery and return to work within 1 to 2 weeks.
Steps You Can Take
If you have any of the symptoms we’ve described and think you may have GERD, contact our office to schedule a complete diagnostic evaluation and discuss both medical and surgical options for effective treatment. Dr. Robert Howard, Dr. Thomas Beetel and Dr. Joseph Levan are all experienced with both workup and treatment of GERD. CLICK HERE to request an appointment online or call our office at 610.375.0500.