In the fight against breast cancer, it may be reassuring to know that they are many effective screening tests in regular use today. When a routine mammogram detects an abnormality, including calcifications within the breast, your doctor may order a biopsy to further aid in diagnosis.
Which Biopsy For My Situation?
There are different types of breast biopsies, and your doctor will choose the biopsy best suited for your care. Generally the type of biopsy used depends on whether a lump can be felt, or if a previous mammogram showed a change within the breast. In many cases, however, a minimally invasive stereotactic breast biopsy may be utilized for its many benefits.
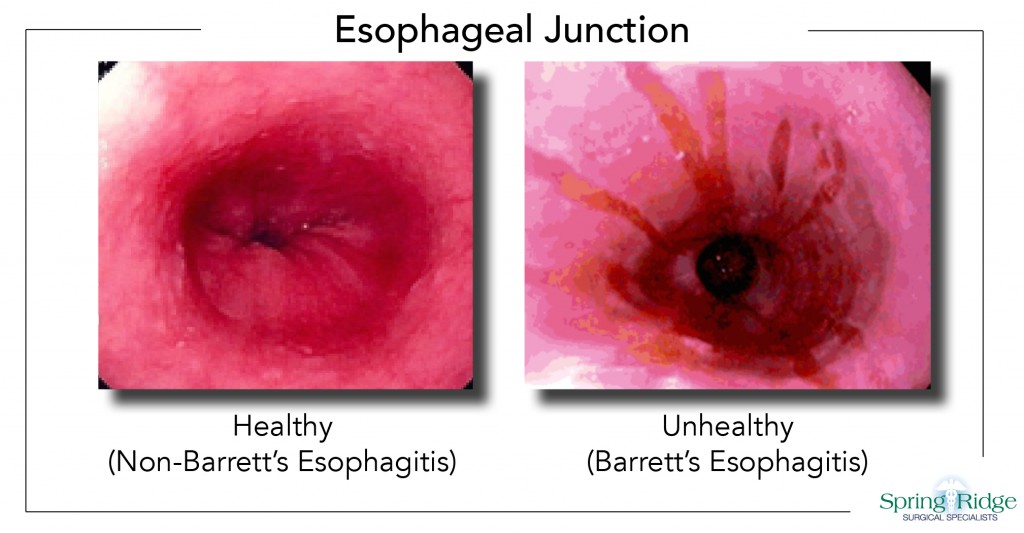
A stereotactic biopsy is an x-ray based, image-guided process that assists the doctor in pinpointing the area of concern, from which a small tissue sample is collected for examination and final diagnosis.
What Can I Expect?
When making your appointment for a biopsy, it’s always a good idea to ask how long the procedure is expected to take. As with any procedure, it may be comforting to have a friend or family member accompany you to the appointment and wait for you until the procedure is completed. For the procedure you’ll either lie down or sit upright, depending on the imaging equipment used.
Just like a mammogram, on the day of the biopsy don’t wear perfume, deodorant, lotion, or put anything else on your skin. This is so the imaging equipment will be able to accurately view the area of concern. A numbing agent will be used on the breast area so you won’t feel any pain. Again just like a mammogram, the breast is compressed between two plates to x-ray the targeted area. A small tissue sample is then taken for examination.
How Soon Can I Go Home?
A stereotactic breast biopsy is a minimally invasive procedure, so unlike surgical biopsies that require an overnight stay, you are able to go home shortly after the procedure is finished. Once home, you may want to take it easy for 24 hours. Your doctor will provide additional self-care instructions as needed, as well as provide biopsy results once they are available. At all times, you are encouraged to ask as many questions as needed to fully understand the procedure, as well as what to expect both during and after.
Providing complete breast cancer screening, surgery and treatment services, Dr. Joseph Levan, Dr. Robert Howard and Dr. Thomas Beetel of Spring Ridge Surgical Specialists perform stereotactic breast biopsies at Reading Health System, and Penn State Health St. Joseph. Each of our surgeons take pride in making certain patients fully understand their care, and options available to them. If you have any questions pertaining to breast cancer care, please contact Spring Ridge Surgical Specialists at 610.375.0500.